Search
- Page Path
- HOME > Search
Original Article
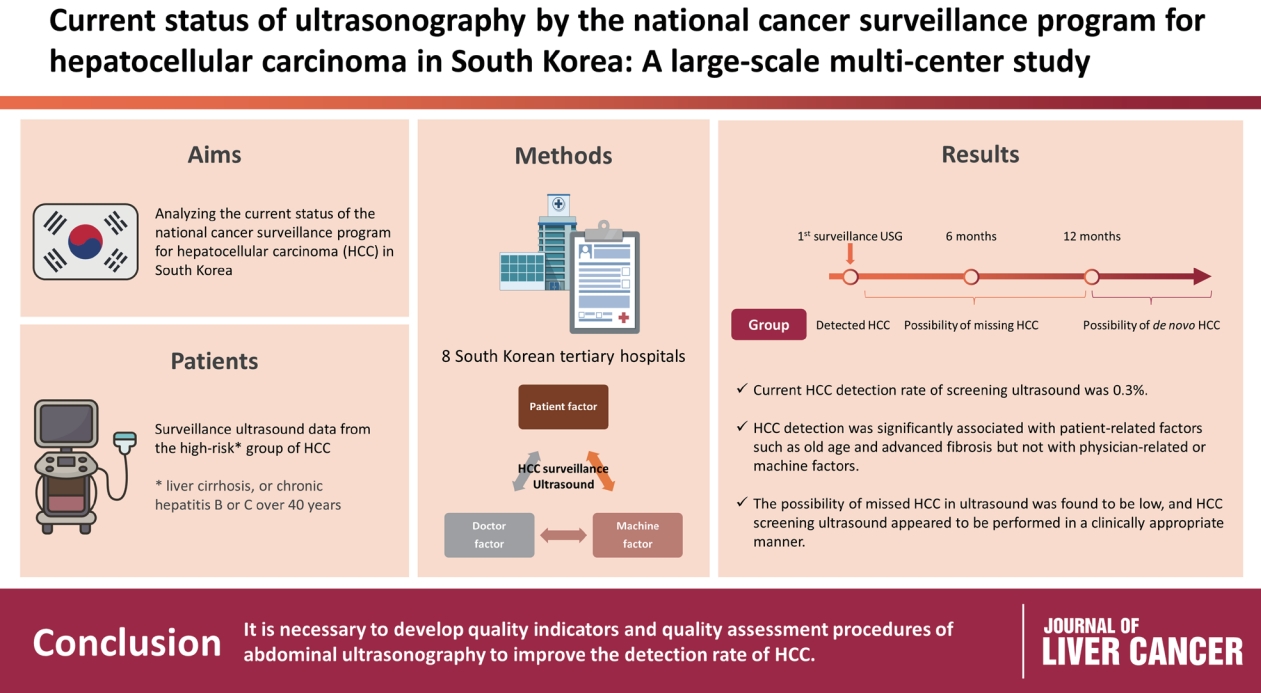
- Current status of ultrasonography in national cancer surveillance program for hepatocellular carcinoma in South Korea: a large-scale multicenter study
- Sun Hong Yoo, Soon Sun Kim, Sang Gyune Kim, Jung Hyun Kwon, Han-Ah Lee, Yeon Seok Seo, Young Kul Jung, Hyung Joon Yim, Do Seon Song, Seong Hee Kang, Moon Young Kim, Young-Hwan Ahn, Jieun Han, Young Seok Kim, Young Chang, Soung Won Jeong, Jae Young Jang, Jeong-Ju Yoo
- J Liver Cancer. 2023;23(1):189-201. Published online March 24, 2023
- DOI: https://doi.org/10.17998/jlc.2023.03.11
- 1,596 Views
- 65 Downloads
- 2 Citations
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background/Aim
Abdominal ultrasonography (USG) is recommended as a surveillance test for high-risk groups for hepatocellular carcinoma (HCC). This study aimed to analyze the current status of the national cancer surveillance program for HCC in South Korea and investigate the effects of patient-, physician-, and machine-related factors on HCC detection sensitivity.
Methods
This multicenter retrospective cohort study collected surveillance USG data from the high-risk group for HCC (liver cirrhosis or chronic hepatitis B or C >40 years of age) at eight South Korean tertiary hospitals in 2017.
Results
In 2017, 45 experienced hepatologists or radiologists performed 8,512 USG examinations. The physicians had a mean 15.0±8.3 years of experience; more hepatologists (61.4%) than radiologists (38.6%) participated. Each USG scan took a mean 12.2±3.4 minutes. The HCC detection rate by surveillance USG was 0.3% (n=23). Over 27 months of follow-up, an additional 135 patients (0.7%) developed new HCC. The patients were classified into three groups based on timing of HCC diagnosis since the 1st surveillance USG, and no significant intergroup difference in HCC characteristics was noted. HCC detection was significantly associated with patient-related factors, such as old age and advanced fibrosis, but not with physician- or machine-related factors.
Conclusions
This is the first study of the current status of USG as a surveillance method for HCC at tertiary hospitals in South Korea. It is necessary to develop quality indicators and quality assessment procedures for USG to improve the detection rate of HCC. -
Citations
Citations to this article as recorded by- The Epidemiology of Hepatitis B Virus Infection in Korea: 15-Year Analysis
Log Young Kim, Jeong-Ju Yoo, Young Chang, Hoongil Jo, Young Youn Cho, Sangheun Lee, Dong Hyeon Lee, Jae Young Jang
Journal of Korean Medical Science.2024;[Epub] CrossRef - Long-Term HBsAg Titer Kinetics with Entecavir/Tenofovir: Implications for Predicting Functional Cure and Low Levels
Soon Kyu Lee, Soon Woo Nam, Jeong Won Jang, Jung Hyun Kwon
Diagnostics.2024; 14(5): 495. CrossRef
- The Epidemiology of Hepatitis B Virus Infection in Korea: 15-Year Analysis

Case Reports
- A case report of a patient presented with skin ulcer after treatment of lenvatinib
- Serin Cha, Dong Woo Kim, Jung Wan Choe, Tae Hyung Kim, Seung Young Kim, Jong Jin Hyun, Sung Woo Jung, Ja Seol Koo, Young Kul Jung, Hyung Joon Yim
- J Liver Cancer. 2021;21(2):194-198. Published online September 30, 2021
- DOI: https://doi.org/10.17998/jlc.2021.09.20
- 3,297 Views
- 78 Downloads
- 1 Citation
-
 Abstract
Abstract
 PDF
PDF - A 60-year-old man diagnosed with unresectable hepatocellular carcinoma (HCC) presented to the hospital with pain in the perineal region. He had been taking lenvatinib every day for 2 months after he was diagnosed with HCC with metastases to the lymph node, small bowel mesentery, and retroperitoneal space. Enhanced abdominal computed tomography revealed mild elevation in intensity in the perineal subcutaneous tissue with subcutaneous emphysema. The patient was diagnosed with Common Terminology Criteria for Adverse Events grade 3, skin ulceration of stage IV with full-thickness skin loss and tissue necrosis in the muscular layer. The patient was taken off the medication with prescription of antibiotics, and after 3 weeks, the skin has fully recovered. This is the first report of an HCC patient who presented with a skin ulceration of stage IV after lenvatinib treatment. We recommend stopping the medication immediately and changing to alternative treatments with appropriate supportive care.
-
Citations
Citations to this article as recorded by- Multiple lenvatinib‐associated skin ulcers: A case report and literature review
Soo Hyun Jeon, Woo Jin Lee, Chong Hyun Won, Sung Eun Chang, Mi Woo Lee, Joon Min Jung
Australasian Journal of Dermatology.2023;[Epub] CrossRef
- Multiple lenvatinib‐associated skin ulcers: A case report and literature review

- Sorafenib-induced Pancreatic Pseudocyst in a Patient with Advanced Hepatocellular Carcinoma: a Rare Adverse Event
- Dae-ha Kim, Minkoo Kim, Hyung Joon Yim, Sang Jun Suh, Young Kul Jung
- J Liver Cancer. 2019;19(2):154-158. Published online September 30, 2019
- DOI: https://doi.org/10.17998/jlc.19.2.154
- 3,449 Views
- 47 Downloads
-
 Abstract
Abstract
 PDF
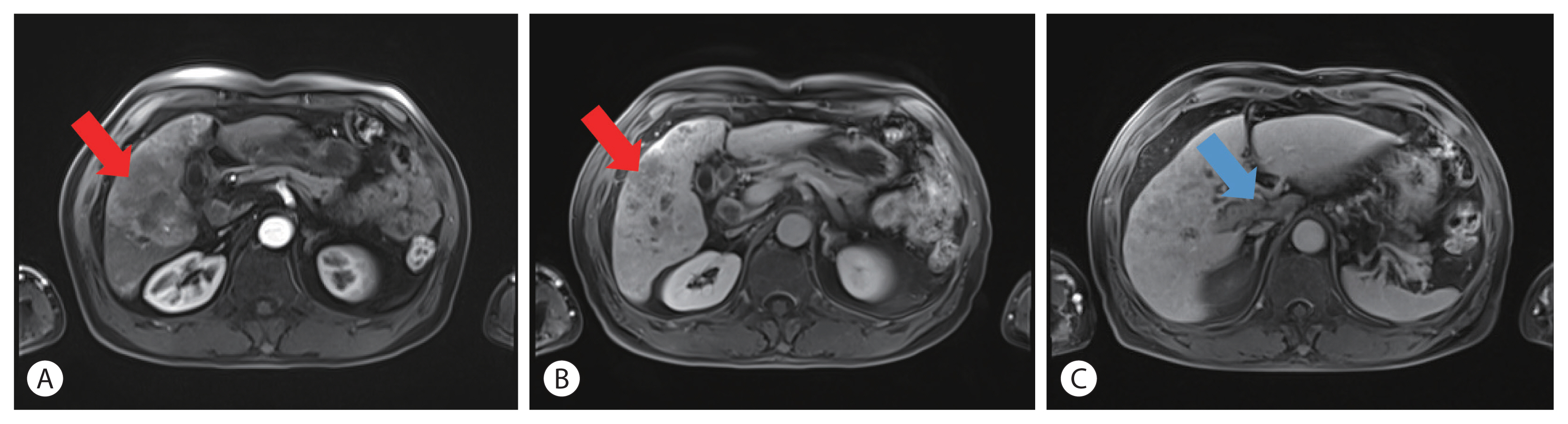
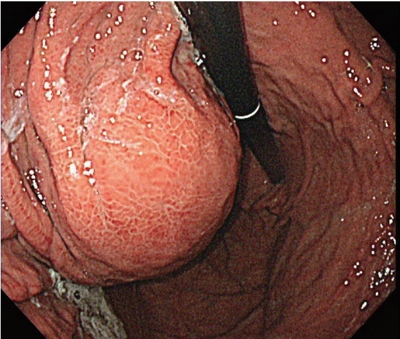
PDF - A 54-year old man diagnosed with advanced hepatocellular carcinoma began treatment with sorafenib. After 3 weeks of treatment, he complained of abdominal pain and nausea. Abdominal sonography showed multiple hepatic lesions only. Serum amylase and lipase levels were 35 U/L and 191 U/L, respectively. The patient was diagnosed with sorafenib-induced acute pancreatitis. After 10 days of discontinuing sorafenib he still complained of nausea and loss of appetite. Esophagogastroduodenoscopy showed a large bulging lesion, which was suspected to cause extrinsic compression on the high body of the gastric anterior wall. Computed tomography scan revealed a cystic lesion, 8.3 cm in size, in the pancreatic tail, suggesting a pancreatic pseudocyst. After the withdrawal of sorafenib, systemic chemotherapy with Adriamycin and cisplatin was administered. Four months after the discontinuation of sorafenib, the size of the pancreatic pseudocyst decreased from 8.3 cm to 3 cm. The patient's symptoms were also relieved.

Original Articles
- An Analysis for Survival Predictors for Patients with Hepatocellular Carcinoma Who Failed to Sorafenib Treatment in Pre-regorafenib Era
- Chan Uk Lee, Young-Sun Lee, Ji Hoon Kim, Minjin Lee, Sehwa Kim, Young Kul Jung, Yeon Seok Seo, Hyung Joon Yim, Jong Eun Yeon, Kwan Soo Byun
- J Liver Cancer. 2019;19(2):117-127. Published online September 30, 2019
- DOI: https://doi.org/10.17998/jlc.19.2.117

- 4,224 Views
- 64 Downloads
-
 Abstract
Abstract
 PDF
PDF - Background/Aim
s: Sorafenib is the standard treatment for patients with advanced hepatocellular carcinoma (HCC). We aimed to investigate the prognosis predictors and the role of second-line cytotoxic systemic chemotherapy (CSC) in patients with advanced HCC after sorafenib discontinuation in the pre-regorafenib era.
Methods
From 2007 to 2015 in the pre-regorafenib era, the medical records of 166 HCC patients, who had permanently discontinued sorafenib, were retrospectively reviewed. For further analysis of survival factors after sorafenib treatment failure, we compared the survival of patients who had maintained liver function after second-line treatment with the best supportive care (BSC) group and selective BSC (SBSC) group.
Results
After discontinuation of sorafenib, median overall survival (OS) was 2.8 (1.9-3.7) months. The OS in patients who discontinued sorafenib due to adverse effect, progression, and poor clinical condition were 5.5 (2.4-8.6), 5.5 (2.2-8.9), and 0.9 (0.5-1.3) months, respectively (P<0.001). The independent predictive factors of survival after sorafenib failure were serum level of bilirubin and albumin, α-fetoprotein, discontinuation cause, and second-line CSC. In comparison with survival between second-line CSC and BSC group, the CSC group showed better survival outcome compared to the BSC group (10.6 vs. 1.6 months, P<0.001) and SBSC group (10.6 vs. 4.2 months, P=0.023).
Conclusions
The survival after sorafenib failure in patients who discontinued sorafenib due to progression and adverse effects was significantly better than in those who discontinued treatment due to clinical deterioration. In the pre-regorafenib era, patients who received second-line CSC showed better survival than those who received only supportive care after sorafenib failure.

- Factors Affecting Prognosis of Hepatocellular Carcinoma with Portal Vein Tumor Thrombosis: Implications for Future Therapeutic Strategies
- Sang Jun Suh, Hyung Joon Yim, Dong Won Lee, Jong Jin Hyun, Young Kul Jung, Ji Hoon Kim, Yeon Seok Seo, Jong Eun Yeon, Kwan Soo Byun, Soon Ho Um
- J Liver Cancer. 2017;17(1):60-71. Published online March 31, 2017
- DOI: https://doi.org/10.17998/jlc.17.1.60
- 2,124 Views
- 23 Downloads
- 1 Citation
-
 Abstract
Abstract
 PDF
PDF - Background/Aim
s: Hepatocellular carcinoma (HCC) with portal vein tumor thrombosis (PVTT) exhibits poor prognosis. The aim of this study is to evaluate factors associated with survival of HCC patients with PVTT to suggest better therapeutic options.
Methods
Patients with HCC which were newly diagnosed at three tertiary hospitals between January 2004 and December 2012, were reviewed retrospectively. Among them, Barcelona Clinic of Liver Cancer stage C patients with PVTT were identified. Factors affecting overall survival (OS) were analyzed and efficacies of the treatment modalities were compared.
Results
Four hundred sixty five patients with HCC and PVTT were included. Liver function, tumor burden, presence of extrahepatic tumor, alfa fetoprotein, and treatment modalities were significant factors associated with OS. Treatment outcomes were different according to the initial modalities. OS of the patients who received hepatic resection, radiofrequency ablation (RFA), transarterial chemoembolization (TACE), hepatic arterial infusion chemotherapy (HAIC), sorafenib, systemic cytotoxic chemotherapy, radiation therapy (without combination), and supportive care were 27.8, 7.1, 6.7, 5.3, 2.5, 3.0, 1.8, and 0.9 months, respectively (P<0.001). Curative-intent treatments such as hepatic resection or RFA were superior to noncurativeintent treatments (P<0.001). TACE or HAIC was superior to sorafenib or systemic chemotherapy (P<0.001). Combining radiotherapy to TACE or HAIC did not provide additional benefit on OS (P=0.096).
Conclusions
Treatment modalities as well as baseline factors significantly influenced on OS of HCC patients with PVTT. Whenever possible, curative intent treatments should be preferentially considered. If unable, locoregional therapy would be a better choice than systemic therapy in HCC patients with PVTT. -
Citations
Citations to this article as recorded by- Value of surgical resection compared to transarterial chemoembolization in the treatment of hepatocellular carcinoma with portal vein tumor thrombus: A meta-analysis of hazard ratios from five observational studies
Keera Kang, Sung Kyu Song, Chul-Woon Chung, Yongkeun Park
Annals of Hepato-Biliary-Pancreatic Surgery.2020; 24(3): 243. CrossRef
- Value of surgical resection compared to transarterial chemoembolization in the treatment of hepatocellular carcinoma with portal vein tumor thrombus: A meta-analysis of hazard ratios from five observational studies

Case Reports
- A Case of Successful Hepatic Resection after Insufficient Response to Transarterial Chemoembolization and Radiation Therapy in Hepatocellular Carcinoma with Portal Vein Invasion
- Seong Kyun Na, Hyung Joon Yim, Sang Jun Suh, Young Kul Jung
- J Liver Cancer. 2016;16(2):118-122. Published online September 30, 2016
- DOI: https://doi.org/10.17998/jlc.16.2.118
- 927 Views
- 5 Downloads
-
 Abstract
Abstract
 PDF
PDF - Hepatocellular carcinoma (HCC) with portal vein invasion has a poor prognosis. Treatments such as transarterial chemoembolization (TACE), radiation therapy (RT), sorafenib are done as a first line treatment. But in case of incomplete response to first line treatment, there’s no established guideline about salvage treatment. We present a 47 year-old male who was diagnosed as HCC with portal vein invasion. He was treated with RT and repeated TACE, but remnant viable tumor was observed. Surgical resection was performed as a salvage treatment, and HCC was completely removed. He has been followed up over 3 years, but there was no recurrence.

- Regression of Advanced Hepatocellular Carcinoma with Lung Metastasis in Response to Sorafenib
- Dae-ha Kim, Gee ho Min, Dong-won Lee, Ke Ryun Ahn, Ji Hye Kim, Snag-Jun Suh, Young Kul Jung, Hyung Joon Yim
- J Liver Cancer. 2016;16(1):57-62. Published online March 31, 2016
- DOI: https://doi.org/10.17998/jlc.16.1.57
- 1,053 Views
- 6 Downloads
-
 Abstract
Abstract
 PDF
PDF - Sorafenib is a multi-targeted tyrosine kinase inhibitor that inhibits Raf kinase and the vascular endothelial growth factor receptor intracellular kinase pathway and is the first agent to demonstrate a statistically significant improvement in overall survival for patients with advanced hepatocellular carcinoma (HCC). However, there were few cases of partial or complete response reported in the previous studies. We herein report a case of dramatic partial response in a patient who had advanced HCC with multiple lung metastasis and portal vein thrombosis treated with sorafenib.

- A Case Report of Transarterial Chemoembolization and Stereotactic Radiation Therapy before Liver Transplantation in a Decompensated Cirrhosis with Hepatocellular Carcinoma
- Sang Hoon Kim, Joo Hee Park, Sang Jun Suh, Young Kul Jung, Hyung Joon Yim
- J Liver Cancer. 2014;14(2):135-138. Published online September 30, 2014
- DOI: https://doi.org/10.17998/jlc.14.2.135
- 944 Views
- 4 Downloads
-
 Abstract
Abstract
 PDF
PDF - Liver transplantation is the only curable treatment modality for hepatocellular carcinoma with advanced liver cirrhosis. While treatment outcome of the liver transplantation is improving, time needed to standby until the surgery is getting longer because of both the lack of liver donors and increasing demands for the transplantation. Therefore, importance of bridging therapy before the liver transplantation is recently highlighted. We herein report our recent experience about a patient who successfully undergone transarterial chemoembolization (TACE) and stereotactic radiation therapy (START) as bridging therapy and later had liver transplantation operation. (J Liver Cancer 2014;14:135-138)

- A Case of Successful Treatment by Radiofrequency Ablation for Pulmonary Metastasis of Hepatocellular Carcinoma
- Jae Chan Park, Yun Soo Kim, Young Kul Jung, Myung Hee Kang, Oh Sang Kwon, Duck Joo Choi, Yang Suh Ku, Ju Hyun Kim
- Journal of the Korean Liver Cancer Study Group. 2013;13(1):51-56. Published online February 28, 2013
- DOI: https://doi.org/10.17998/jlc.13.1.51
- 3,668 Views
- 7 Downloads
-
 Abstract
Abstract
 PDF
PDF - Surgical resection or liver transplantation is a main curative modality for hepatocellular carcinoma (HCC). But nowadays local ablation therapy is being accepted as a useful option for local control therapy for HCC. Here we present a case of 59 years old male with hepatitis B virus related liver cirrhosis, who underwent surgery for HCC at S6 two years ago. He had received percutaneous ethanol injection (PEI), radiofrequency ablation (RFA) and multiple sessions of transarterial chemoembolization (TACE) for intrahepatic recurrences of HCC after surgery. A small radio-opaque lesion occurred at the left upper lobe of lung. Metastatic HCC was confirmed by CT-guided percutaneous needle core biopsy. CT-guided RFA for pulmonary metastasis was performed. Now it is been 11 months after the treatment without any recurrence.

Review Article
- Management of Cirrhotic Complications in Hepatocellular Carcinoma: Portal Hypertension, Ascites, and Variceal Beeding
- Young Kul Jung, Duck Joo Choi
- Journal of the Korean Liver Cancer Study Group. 2012;12(2):85-87. Published online September 30, 2012
- 963 Views
- 56 Downloads
-
 Abstract
Abstract
 PDF
PDF - Hepatocellular carcinoma (HCC) causes approximately one million deaths every year. Due to advanced stage at diagnosis, HCC carries a five-year survival rate of less than 5%, if diagnosed with unresectable disease. And also HCC is responsible for significant morbidity and mortality in cirrhosis. It leads to decompensation of cirrhosis and is the cause of death in up to 25% of cirrhotic patients. The purpose of this article is to provide an overview of the complexity in complication management of patients with terminal stage of HCC. The occurrence of complications in HCC patients is common, and includes portal hypertension, ascites, and variceal bleedings. Because of the limitations in the efficacy of current treatment options for terminal stage HCC, complication management is a key to preserving physical functioning and quality of life in these patients. Until now, diuretics remain the gold standard in management of ascites in cancer patients, and endoscopic treatment and vasoconstrictor are good choice for acute variceal bleedings. In several studies, sorafenib showed a potential as therapeutics for portal hypertension in patients with advanced HCC.

Case Reports
- A Case of Small Hepatocellular Carcinoma Less Than 1 cm
- Yun Jeong Jo, Young Kul Jung, Dong Hae Chung, Oh Sang Kwon, Yun Soo Kim, Duck Joo Choi, Ju Hyun Kim
- Journal of the Korean Liver Cancer Study Group. 2012;12(1):42-46. Published online February 28, 2012
- 484 Views
- 1 Download
-
 Abstract
Abstract
 PDF
PDF - Hepatocellular carcinoma (HCC) is one of the most important causes of cancer death in South Korea. Approximately two thirds of the patients are diagnosed in the advanced stage with multiple metastasis and underlying liver dysfunction, so they are not suitable to undergo curative resection. Small HCC has no consensus about diagnostic criteria but became known early stage HCC that means good prognosis. Cases of small HCC have been increasing with the progress of diagnostic methods. We experienced a case of incidentally found small HCC less than 1 cm from liver cirrhosis by liver dynamic imaging, so reported it.

- A Case of Improvement of Hypoglycemia by Sorafenib in Hepatocellular Carcinoma
- Kwang Il Ko, Young Kul Jung, Jungsuk An, Oh Sang Kwon, Yun Soo Kim, Duck Joo Choi, Ju Hyun Kim
- Journal of the Korean Liver Cancer Study Group. 2012;12(1):47-50. Published online February 28, 2012
- 524 Views
- 0 Download
-
 Abstract
Abstract
 PDF
PDF - The prevalence of hypoglycemia in hepatocellular carcinoma (HCC) ranged from 4 to 27%. The causes of hypoglycemia in HCC are two type. Type A is a poorly differentiated tumor with mild to moderate severity of hypoglycemia that occurs in the late stage of the disease. The less common type B tumor is a well-differentiated slow growing tumor in which severe hypoglycemia occurs in early stages of the disease. We reported a case of improvement of hypoglycemia due to HCC by sorafenib.


 E-submission
E-submission THE KOREAN LIVER CANCER ASSOCIATION
THE KOREAN LIVER CANCER ASSOCIATION

 First
First Prev
Prev



 Follow JLC on Twitter
Follow JLC on Twitter